Mutations to BRCA can influence an individual’s risk of developing pancreatic cancer and impact treatment decisions for a patient.
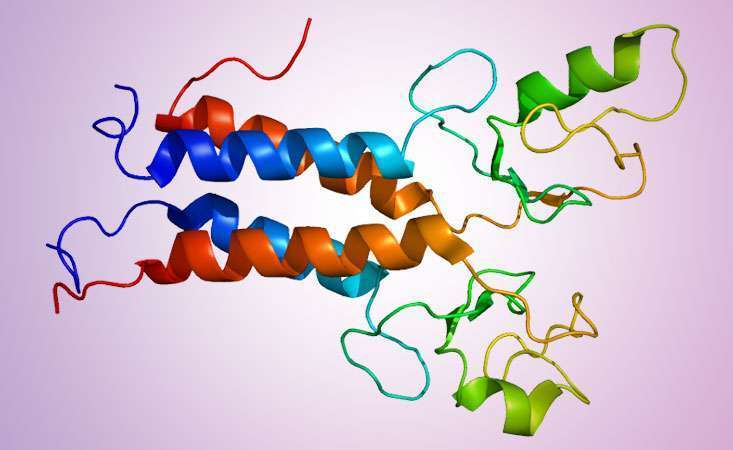
Graphic by Emw (Own work) [CC BY-SA 3.0 or GFDL], via Wikimedia Commons]
Editor’s note: We originally published this blog in 2017. Since then, there have been new developments related to BRCA and pancreatic cancer, so we’ve updated this piece to reflect those changes.
Did you know that mutations in the “breast cancer genes,” BRCA1 and BRCA2, increase a person’s lifetime risk of developing breast, ovarian AND other cancer types, including pancreatic? This can affect both men and women. In conjunction with Breast Cancer Awareness Month, and in preparation for Pancreatic Cancer Awareness Month in November, check out five important facts about BRCA mutations and how they impact pancreatic cancer risk as well as influence treatment options.
- BRCA proteins impact cells’ ability to repair DNA damage. The BRCA genes (BRCA1 and BRCA2) are tumor suppressor genes, which means that they prevent healthy cells from becoming cancerous. Their normal function is to repair damage to DNA, but when BRCA1 or BRCA2 is mutated and doesn’t work correctly, the accumulation of unrepaired DNA damage can ultimately lead to unregulated cell growth, or cancer.
- BRCA mutations increase a person’s risk of several cancer types, including pancreatic. All genes exist in the body in pairs – meaning that you inherit one copy (or version) from each parent. People can be born with one healthy and one mutated version of BRCA, leading to an increased (but not certain) lifetime cancer risk. Cancer could develop only if the second, healthy copy of the BRCA1 or BRCA2 gene gets mutated or altered, which could happen due to an environmental exposure (like smoking) or a mistake in the cellular genetic machinery.
- Ashkenazi Jews have a higher rate of BRCA mutations than the general American population. It is thought that around one in 40 individuals of Ashkenazi Jewish descent carry a BRCA1 or BRCA2 mutation. By contrast, studies have suggested that BRCA mutations occur in the range of one in 400 to one in 800 within the general non-Ashkenazi Jewish population.
- Genetic counselors and screening programs can help determine and monitor risk. Genetic testing may reveal mutations (like BRCA) and help inform family members of risk, regardless of family history. PanCAN recommends all pancreatic cancer patients receive genetic testing for inherited mutations, as well as genetic counseling. Guidelines also recommend genetic counseling for those with other cancer types often linked to BRCA mutations. If you are a first-degree relative (parent, child or sibling) of someone with pancreatic cancer, you may benefit from genetic counseling and genetic testing as well. Recent evidence suggests that individuals at high genetic risk for pancreatic cancer whose tumor is found through a surveillance program are diagnosed at an earlier stage and live longer than people whose cancer is found outside of a surveillance program.
- For those with cancer, mutations to BRCA can inform and improve treatment. Evidence suggests that cancer cells with BRCA mutations may respond particularly well to a certain type of chemotherapy as well as a targeted therapy called PARP inhibition. The PARP inhibitor Lynparza® (olaparib) was approved for patients with metastatic pancreatic cancer, who have BRCA1 or BRCA2 mutations, and whose tumor previously responded to platinum-based chemotherapy.
Every pancreatic tumor is different, and patients who receive treatment based on their biology can live longer. PanCAN strongly recommends genetic testing for inherited mutations and biomarker testing of your tumor to help determine the best treatment options.

Alison Klein, MHS, PhD
“Knowledge of a germline (inherited) BRCA1 or BRCA2 mutation can affect an entire family, not just an individual,” said Alison Klein, MHS, PhD, professor of oncology, pathology and epidemiology at Johns Hopkins University, and member of PanCAN’s Scientific and Medical Advisory Board. “It’s important to consult with a genetic counselor to determine who should be tested and to understand how to interpret results.”
Klein continued: “The more we learn about the genetics of pancreatic cancer, the more complexity we uncover. It’s important for people to know their family history so they can understand their risk of developing pancreatic and other cancer types, and to know the genetic features of their tumor, so that they can be aware of treatment options that might be best for them.”















