Michael Goggins, MD
For over two decades, Michael Goggins, MD, has been researching how to detect pancreatic cancer at an earlier stage, so that more patients have a better chance at survival.
In 1998, his work inspired PanCAN founder Pamela Acosta Marquardt to host the first “An Evening with the Stars” gala, with proceeds to benefit a lab he wanted to create at Johns Hopkins University – the first lab in the country dedicated to early detection research for pancreatic cancer.
Without that support, he said at the time, he may not have been able to get the lab off the ground. The gala gave him the funds he needed to set a research agenda and bring together a team.
Fast forward to 2013, when Dr. Goggins received one of the first $1 million Research Acceleration Network (RAN) Grants from PanCAN, established in memory of Skip Viragh, providing his lab with three years of funding to maintain and expand his work.
Now, nine years later as the Sol Goldman Professor of Pancreatic Cancer Research at Johns Hopkins Medicine, Dr. Goggins is a leader in the field. Over time, his research has continued to yield a better understanding of how to improve survival through early detection.
His lab’s most recent publication in the Journal of Clinical Oncology made news for its definitive findings: Regular screening of a high-risk population confers substantial survival benefits.
“The overall survival of patients who maintained surveillance recommendations, which is generally annual surveillance, was approximately 10 years,” he said. “Which really equates to long-term survival and hopefully – cured.”
The paper focuses on findings from the Cancer of Pancreas Screening 5 study, known as CAPS5. To enroll, individuals must have either a germline genetic mutation associated with higher risk of pancreatic cancer, such as BRCA 1 and 2 or PALB2, or at least one first-degree and one second-degree relative diagnosed with pancreatic cancer. There was also an age requirement. Participants went through annual surveillance to detect pancreatic cancer, either through endoscopic ultrasound or MRI.
The results were “dramatic” in terms of long-term survival benefit, said Dr. Goggins.
“The majority of patients who maintain surveillance were diagnosed with stage I disease. And indeed, in the CAPS5 study, that was more like three quarters,” he said. “Stage I disease does equate very well with long-term survival.”
CAPS5 has been enrolling participants since 2014 and it builds on four previous cohorts, CAPS1-CAPS4, that date back to 1998. That 20-plus years of data – including more than 1,700 participants – has yielded consistent findings: Routine screening of high-risk individuals results in a higher number stage I diagnoses as compared to those with no screening. This provides additional treatment options, leading to improved long-term survival.
These striking results are the product of decades of research.
“The CAPS study had a different goal when we started over 20 years ago,” said Dr. Goggins. “First, it was focused on whether you could even do early detection successfully in the highest risk people. And then, as we started to see benefits, we focused on how good the benefits were. Then we asked the question, ‘What is the best strategy?’”
Looking ahead, Dr. Goggins sees opportunities to dive more deeply into how to recognize high-risk individuals as well as get the word out about the importance of routine screening for this population.
“It’s a major effort over many years to try and identify who’s at risk and get them into these programs, whether it’s through genetic testing or family history,” he said. “I know PanCAN is a key player in that effort.”
He cites PanCAN’s Early Detection Initiative, which is focused on studying sudden-onset diabetes as a risk factor for pancreatic cancer, as one important study that aims to identify who among this group has pancreatic cancer.
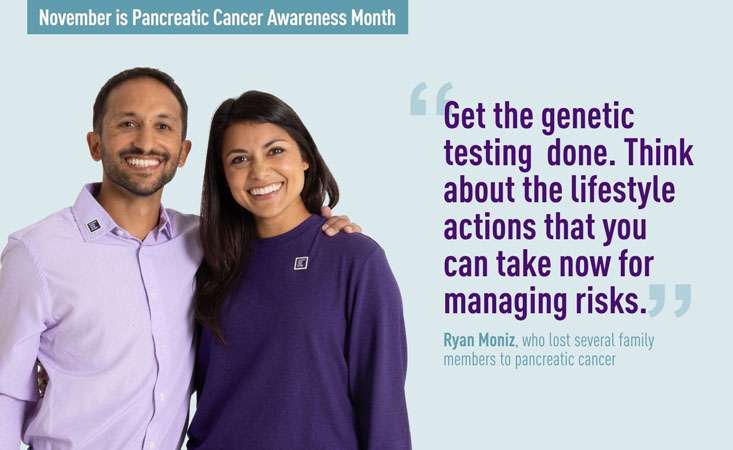
One notable change over time: Dr. Goggins is buoyed by the uptick in individuals getting genetic testing to understand their inherited risk for pancreatic cancer.
“One of the trends that has occurred in recent years is a greater percentage of the CAPS study population, the people who are coming to see us, are coming with referrals because they have a germline mutation in one of the pancreatic cancer susceptibility genes,” he said. “Once upon a time, it was under a quarter, or under a third of who we had enrolled. Now, it’s basically approaching half.”
As these efforts yield more individuals looking for routine surveillance, one of the next challenges becomes justifying the tests to offset the costs to patients.
“We are now working with some of our advocates trying to get more uniform approval and insurance coverage for these kinds of tests because there’s a lot of need,” he said. “We’re hoping that these long-term studies will lead to accelerated progress.”
Another potential future study topic hinges on understanding why some high-risk individuals don’t continue with routine screening and what could be done to keep them engaged.
“We need to try and understand the barriers,” he said. “Why do some people drop off and what are those factors? What impacts compliance?”
He’s optimistic that progress will be made on all of these fronts in part because of the incredible network of researchers that has come together since the late 1990s. They’re focused on all aspects of the disease, driven in part by PanCAN’s investment in research funding, $174 million to date. He points to everything from the Career Developments Awards – important to build a pipeline of young researchers – to PanCAN’s annual Scientific Summit as key reasons why the field is now so robust.
“The field of pancreatic cancer research has exploded compared to when I was starting,” he said. “And the diversity of expertise that we can bring to a project, the number of disciplines and the number of investigators, makes it an exciting area to work in. We’re all trying to figure out the most important findings and translate them into patient care and patient advances. PanCAN has helped to do that, for sure.”