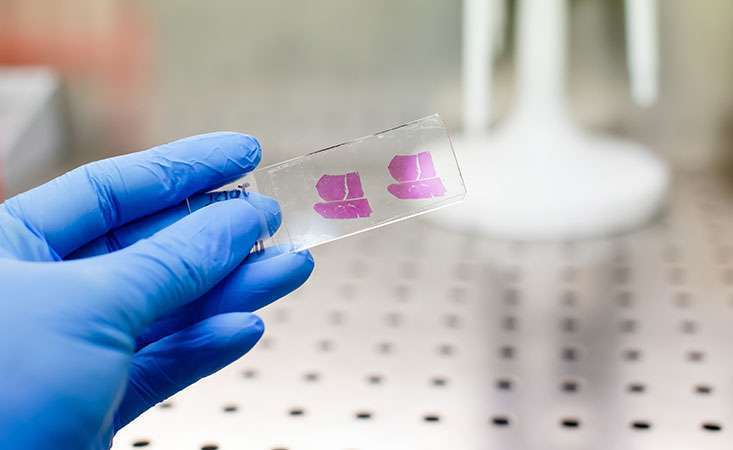
Researchers evaluated whether tumor tissue from the pancreas or metastatic site is preferred for molecular profiling.
When the Pancreatic Cancer Action Network (PanCAN) launched its Know Your Tumor® precision medicine service, molecular profiling was offered for pancreatic cancer tissue samples that came from a patient’s primary tumor in the pancreas or from metastatic sites, such as the liver or lung.
Published yesterday in the British Journal of Cancer, PanCAN and its partners, led by Perthera, Inc., presented results suggesting both sources of tissue samples provide equally meaningful information for patients and their healthcare teams.
“Our findings are in agreement with and expand upon previous studies suggesting an adequate pancreatic cancer tissue sample from the primary tumor or metastatic site can be informative for molecular profiling through Know Your Tumor,” said Lynn Matrisian, PhD, MBA, PanCAN’s chief science officer and a co-author of the study. “We believe this finding will make the molecular profiling process more accessible and convenient for patients.”
Molecular profiling provides a detailed report of the biological characteristics unique to that patient’s cancer cells. And, this information may be able to guide treatment decisions.
Every pancreatic tumor is different. PanCAN strongly recommends molecular profiling of your tumor to help determine the best treatment options.
PanCAN and its partners previously published results from Know Your Tumor, showing improved outcomes for patients whose treatment was aligned with their tumor’s biology.
In the current study, the research team looked at reports from 713 different patients with pancreatic adenocarcinoma, the most common form of the disease. Of these, 282 samples came from patients’ primary tumors (from diagnostic biopsy or a surgical specimen), 278 samples came from liver metastases and 54 from the lung or thoracic cavity. The remaining tumor tissue samples came from other locations within the abdomen.
“It’s important to note that, in nearly all the cases, we did not look at samples from the primary tumor and metastatic tumor of the same patient, side by side,” Matrisian cautioned. “This would provide a more definitive answer whether the same molecular changes appear in the primary tumor as well as cancer cells that have spread.”
However, the study showed nearly identical patterns of genetic changes in the groups of samples taken from patients’ primary tumors vs. various metastatic sites.
This finding is different from other cancer types, Matrisian noted. “In other tumor types, like breast, prostate, lung or colorectal, it’s been well established that the genetic characteristics of cells from the primary tumor and the metastatic site are different.”
She continued, “This happens because the cancer cells in these primary tumors need to accumulate additional mutations and other changes to become aggressive enough to spread. Unfortunately, in the case of pancreatic cancer, we believe most cells within the primary tumor are very aggressive and already have the potential to metastasize.”
Finally, the research team closely evaluated “highly actionable” alterations – those with significant clinical evidence in pancreatic cancer or other cancer types that a certain type of treatment may be particularly beneficial. Again, the evidence suggested a similar rate and pattern of highly actionable alterations present in either cancer cells from the primary tumor or metastatic site.
“Based on these results, whether a patient has a tissue sample available from their initial diagnosis, from a sample obtained during surgery or from a biopsy of a metastatic site – any of these samples can provide meaningful information that may help guide treatment decisions,” Matrisian said.
“We’re grateful to the patients who have enrolled in Know Your Tumor – we’ve delivered personalized reports to more than 1,000 pancreatic cancer patients to date. And we’re pleased to continue to contribute findings to the field about the benefits of molecular profiling for pancreatic cancer patients.”














